Neurological conditions affect millions of people globally, with symptoms ranging from mild issues like headaches to more severe diseases such as epilepsy, Parkinson’s disease, Alzheimer’s disease, and multiple sclerosis. These conditions often require specialized care due to the complexity of the nervous system. Neurologists are the specialists trained to diagnose, treat, and manage these disorders. Understanding the role of a neurologist in diagnosing neurological conditions is essential for recognizing when it’s time to seek medical advice and how they can help guide you through the diagnostic process.
What Is a Neurologist?
A neurologist is a medical doctor who specializes in treating disorders that affect the brain, spinal cord, and nerves. Neurologists possess a deep understanding of how the nervous system works and how diseases and injuries disrupt normal function. From chronic headaches and migraines to serious conditions like strokes, neurodegenerative diseases, and epilepsy, neurologists are trained to assess, diagnose, and manage these disorders effectively. Their expertise enables them to understand the complexities of various neurological diseases, allowing them to provide tailored treatments for patients.
The role of the neurologist is crucial because neurological diseases can affect virtually every aspect of bodily function, from motor skills to cognitive abilities. Diagnosing these conditions requires a thorough approach, involving detailed patient history, physical examinations, diagnostic tests, and sometimes advanced imaging techniques.

The Importance of the Initial Consultation
The first step in diagnosing a neurological condition often begins with a detailed consultation. During this session, the neurologist gathers important information about the patient’s symptoms, medical history, and lifestyle. Symptoms such as persistent headaches, dizziness, muscle weakness, or difficulty speaking may all indicate a neurological issue.
In addition to assessing symptoms, the neurologist will ask about any family history of neurological disorders, as many neurological conditions, such as Huntington’s disease or Alzheimer’s, can have a genetic component. The neurologist will also inquire about the patient’s lifestyle, stress levels, exposure to environmental toxins, and any other factors that might contribute to their symptoms. This comprehensive evaluation provides the neurologist with crucial insights to narrow down potential causes.
Neurological Examination: A Thorough Assessment
After the consultation, the neurologist performs a physical neurological examination. This is a critical part of the diagnostic process, helping to assess the function of the nervous system. The exam includes several key tests, such as:
- Motor skills and coordination: The neurologist may ask the patient to perform specific tasks like walking or moving their limbs to assess muscle strength, coordination, and balance. These tests help identify issues with motor skills, which can indicate neurological disorders such as Parkinson’s disease or multiple sclerosis.
- Reflex testing: The neurologist may test deep tendon reflexes by tapping on the knee or elbow. Abnormal reflexes can point to issues in the brain or spinal cord.
- Sensory testing: The neurologist checks for abnormal sensations like numbness or tingling, which could indicate nerve damage or neuropathy.
- Cognitive function: Tests are often conducted to assess memory, reasoning, and problem-solving abilities. This is particularly important for identifying conditions like Alzheimer’s disease or other forms of dementia.
This examination provides the neurologist with important clues that guide the next steps in the diagnostic process.
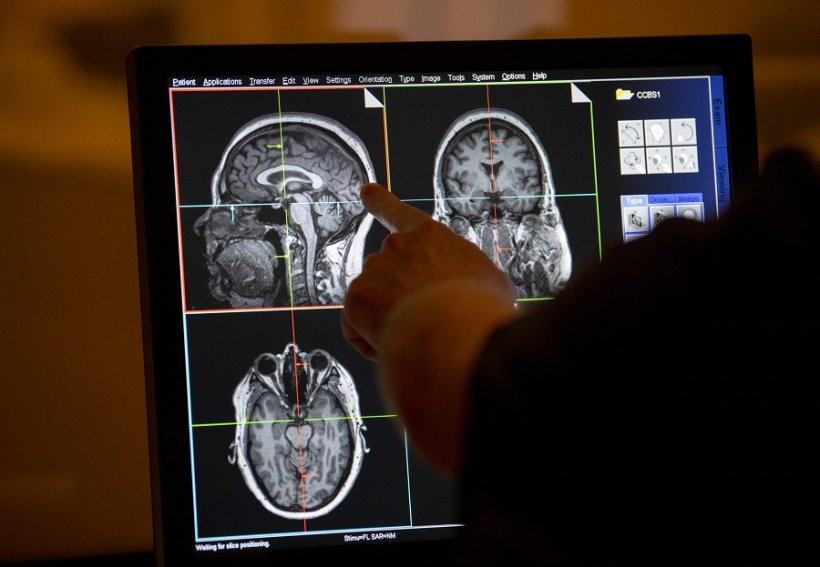
Diagnostic Imaging: Visualizing the Problem
Once the neurological examination is complete, the neurologist may recommend diagnostic imaging tests to further explore the root cause of the symptoms. Imaging techniques, such as MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans, provide detailed images of the brain, spinal cord, and other parts of the nervous system. These tests are crucial in detecting structural issues like tumors, strokes, or degenerative diseases.
An MRI, for example, is particularly useful in identifying changes in soft tissues, such as brain lesions or plaques associated with multiple sclerosis. A CT scan may be used more frequently in emergency situations, such as after a head injury, to check for bleeding or brain swelling. In some cases, a neurologist may also recommend a PET (Positron Emission Tomography) scan to assess brain function and activity, especially when diagnosing conditions like Alzheimer’s disease or other neurodegenerative diseases.
Electrophysiological Tests: Measuring Nerve Activity
In addition to imaging, neurologists often use electrophysiological tests to measure the electrical activity in the brain, spinal cord, and peripheral nerves. These tests help evaluate how well the nervous system is functioning and can identify abnormalities that may not be visible through imaging. Common electrophysiological tests include:
- Electroencephalogram (EEG): This test measures electrical activity in the brain and is frequently used to diagnose epilepsy or other seizure disorders. It can also identify abnormal brainwave patterns associated with conditions like sleep disorders.
- Electromyography (EMG) and Nerve Conduction Studies (NCS): EMG assesses the electrical activity of muscles, while NCS measures how well electrical signals travel through nerves. These tests are used to diagnose conditions like ALS (amyotrophic lateral sclerosis), carpal tunnel syndrome, and peripheral neuropathy.
These tests provide vital information that can help the neurologist determine the location and nature of the neurological problem, making it easier to pinpoint the correct diagnosis.
Genetic Testing and Biomarkers: New Tools in Diagnosis
Genetic testing and biomarkers are emerging tools in the field of neurology that are helping neurologists diagnose hereditary neurological conditions and monitor disease progression. Many neurological disorders, such as Huntington’s disease or familial Alzheimer’s disease, are genetic in nature, and genetic testing can help confirm these diagnoses early.
Biomarkers are also helping to improve diagnosis. These are substances found in blood or cerebrospinal fluid that indicate the presence of neurological diseases. For example, elevated levels of tau proteins are associated with Alzheimer’s disease, while neurofilament light chain proteins can indicate multiple sclerosis. By analyzing these biomarkers, neurologists can diagnose conditions more accurately and track how the disease is progressing.
Treatment Plans: Tailored to the Diagnosis
Once a neurological condition is diagnosed, the neurologist works with the patient to determine the best course of action. Depending on the diagnosis, treatments can vary widely, from medication to lifestyle changes, surgery, or physical therapy. For example, conditions like epilepsy can be treated with anticonvulsants, while those with Parkinson’s disease might benefit from dopamine replacement therapy.
The neurologist’s role also involves providing ongoing care for chronic neurological conditions. Regular follow-up visits are essential to track disease progression, manage symptoms, and adjust treatment plans as needed. Some conditions, like multiple sclerosis or Alzheimer’s disease, require long-term care management to slow disease progression and improve the quality of life for patients.
Ongoing Care and Support
Neurological conditions like multiple sclerosis, epilepsy, and dementia often require ongoing care. Neurologists are responsible for monitoring disease progression and adjusting treatment as necessary. Regular follow-up appointments help track the effectiveness of treatments, manage side effects, and address any new symptoms that may arise.
In some cases, neurologists may work with a team of healthcare providers, including physical therapists, occupational therapists, psychologists, and social workers, to ensure that patients receive holistic care and support.
Conclusion
The role of a neurologist in diagnosing and treating neurological conditions is pivotal in providing patients with effective care. Through a combination of detailed consultations, physical exams, advanced diagnostic tests, and genetic analysis, neurologists are able to accurately diagnose a wide range of neurological issues. Early diagnosis, coupled with timely intervention, is key to managing these conditions and improving patient outcomes. As medical science continues to advance, the tools and methods available to neurologists will continue to evolve, offering new hope and solutions for those living with neurological disorders.













+ There are no comments
Add yours